Introduction — Why the gut immune axis matters more than you think
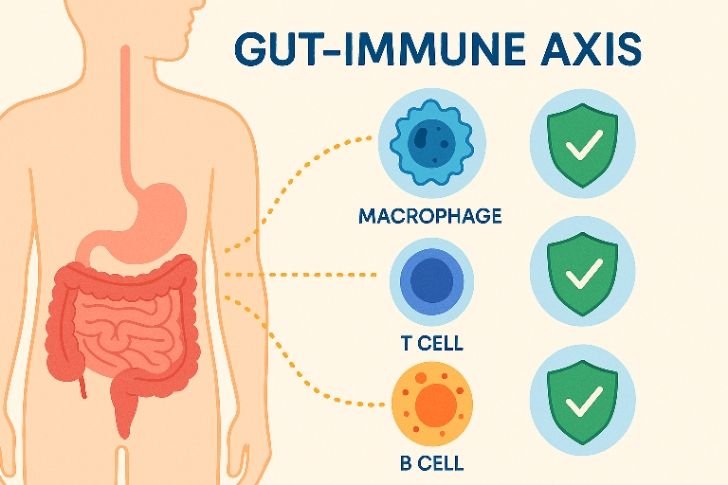
We often think of immunity as something that wakes up only when illness arrive, but actually your immune system is awake all the time — working quietly, checking and re-checking. And the busiest hub for that defense work? The gut. The gut immune axis is the biologic conversation between your digestive tract and the immune system; it is the channel where food, microbes, and immune cells exchange messages every minute of the day.
When the gut immune axis is balanced, inflammation stays in check, pathogens are handled, and recovery is fast. But when that axis is disturbed — by poor diet, chronic stress, antibiotics overuse, or bad sleep — immunity can wobble, leading to more colds, longer recoveries, and sometimes chronic inflammation. In this article we’ll explore what this axis is, why it’s central to health, how to detect trouble, and exactly what to do to strengthen it — practical steps that actually work.
What is the gut immune axis? A plain-language explanation
The gut immune axis is not a single organ or a single hormone — it’s a system. It includes:
the intestinal lining (the barrier),
the microbiome (trillions of bacteria and other microbes),
immune cells in the gut-associated lymphoid tissue (GALT),
and the biochemical signals (cytokines, short-chain fatty acids, neurotransmitters).
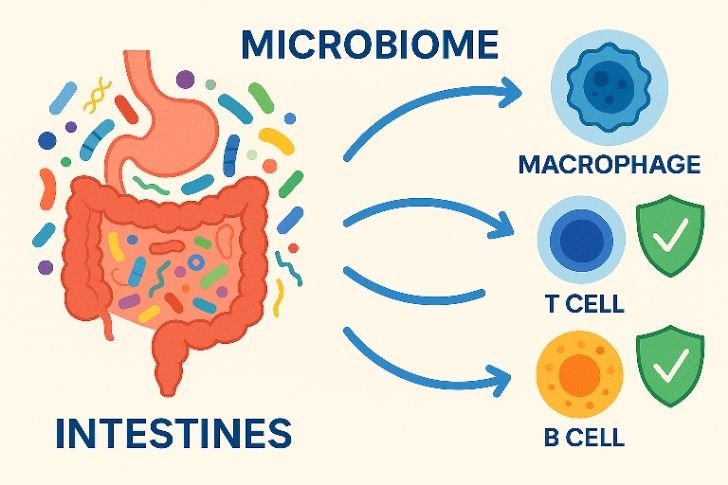
They talk constantly. Microbes produce metabolites that tell immune cells to “calm down” or “gear up.” Immune cells decide whether to tolerate a harmless food molecule or launch a defensive response. The gut immune axis is that two-way street. Think of it like an ongoing neighborhood meeting where the residents (bacteria), the city guards (immune cells), and the road network (intestinal barrier) all coordinate safety and repair.
Why digestive health directly shapes immunity
The microbiome speaks to immunity
Your gut microbiome is like a living orchestra. When the different instruments (microbial species) play in harmony, the immune system hears a balanced symphony. When one instrument overpowers the others (dysbiosis), the music becomes chaotic — and that chaos confuses immune cells.
Healthy microbes produce short-chain fatty acids (SCFAs) such as butyrate and propionate. These compounds soothe inflammation, support the gut barrier cells, and instruct immune cells to behave. The presence of SCFAs is one of the clearest molecular examples of how the gut immune axis actually functions.
The gut barrier is the frontline
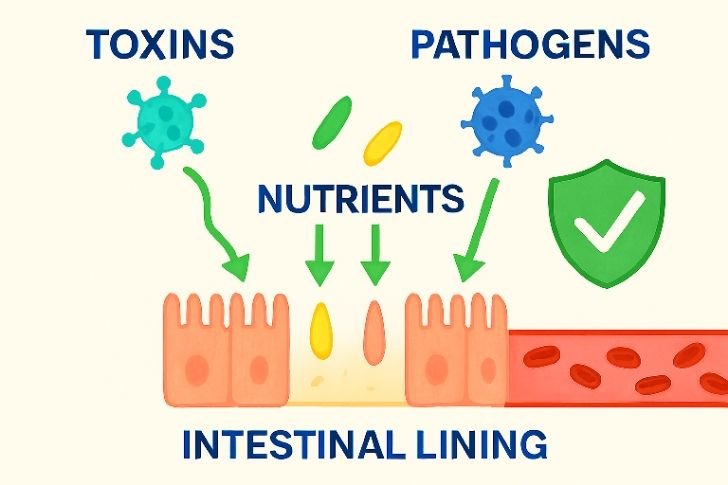
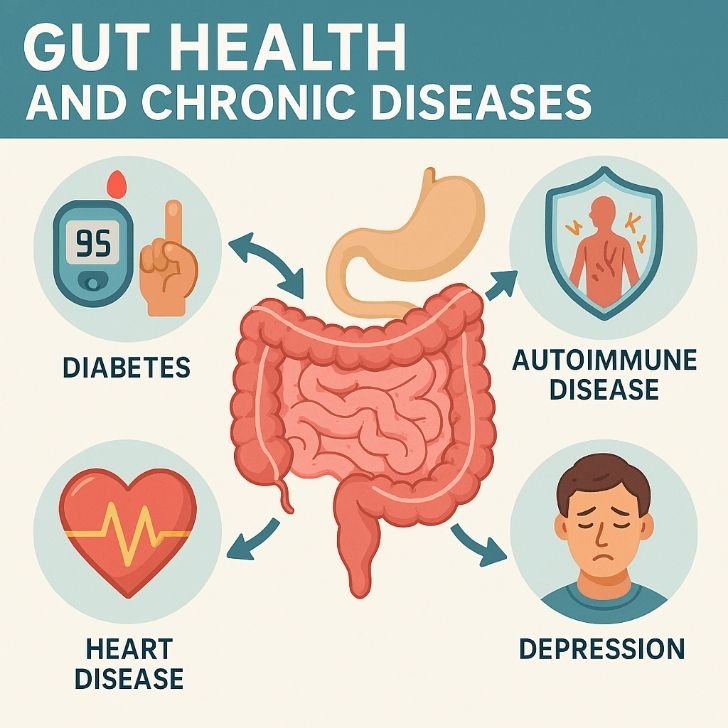
Your intestinal wall is one-cell thick in many places — yet it forms a highly active barrier. This barrier stops toxins and microbes from slipping into the bloodstream. When the barrier becomes more permeable (so-called “leaky gut”), particles cross, immune cells detect them, and the immune system triggers inflammation. That’s the gut immune axis misfiring: the barrier leaks, immunity overreacts, and systemic inflammation follows.
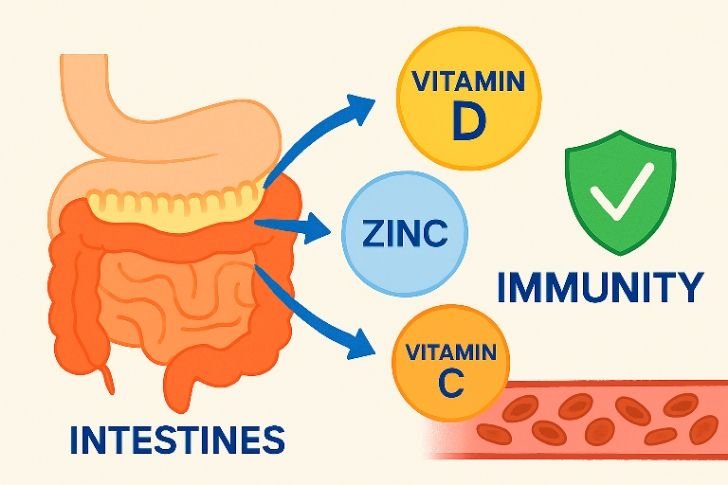
Nutrient absorption fuels immune cells
Immune cells require fuel and micronutrients. Poor digestion or malabsorption reduces availability of vitamin D, zinc, iron, and B-vitamins — all crucial for immune cell function. Thus digestive dysfunction weakens the immune response indirectly but powerfully. This is another key way the gut immune axis influences systemic health.
• Scientists now also describe the gut–brain–immune triangle. The vagus nerve, running from the brain into the gut, carries messages that influence both digestion and immune regulation. Stress or anxiety can shift the nerve’s signals, tightening or loosening the gut barrier, and changing the way immune cells respond.
This is why people under chronic stress often experience both gut discomfort and lowered immunity at the same time. By calming the nervous system through practices like slow breathing, yoga, or meditation, you send positive signals down the vagus nerve.
These signals stabilize the gut immune axis and give immune cells clearer guidance on what is safe and what is threatening. In other words, your mental state is not separate from your digestion—it is another dial that tunes your inner defenses.
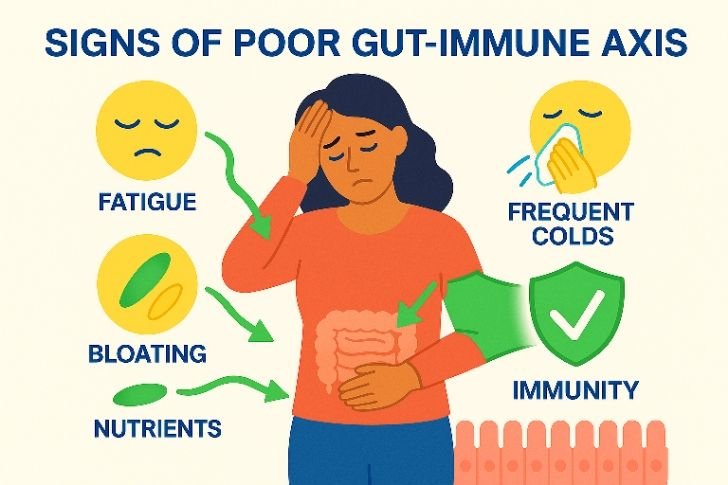
Symptoms and signs of an unhappy gut immune axis
You can’t measure the gut immune axis directly at home, but your body gives clues. Look for patterns:
recurrent infections or slow recoveries
persistent gut symptoms: bloating, gas, irregular stools
food sensitivities that appear suddenly
unexplained fatigue or “brain fog”
autoimmune flare-ups or new inflammatory conditions
mood changes: anxiety, low mood — because the gut makes neurotransmitters
If several of these show up together, the gut immune axis may be unbalanced and deserves attention.
• While you can’t fully diagnose the state of the gut immune axis at home, there are some accessible checks. Simple blood tests, like vitamin D or CRP levels, give clues about systemic inflammation. Food and symptom journals can help reveal patterns between meals and immune flares. Stool tests available online may estimate microbiome diversity, though their accuracy is variable. Even keeping a daily log of energy, digestion, and sleep creates valuable data.
Over time, such records highlight whether your changes—like adding fiber or probiotics—are making a real difference. This practical tracking grounds the abstract concept of the gut immune axis into visible, measurable shifts in your daily life.
Root causes that disrupt the gut immune axis
Many modern habits chip away at this axis slowly:
Poor diet: high sugar, ultra-processed foods, low fiber feed harmful microbes.
Chronic stress: stress hormones like cortisol break down barrier function and reduce microbial diversity.
Sleep loss: circadian disruption changes microbiome rhythms and impairs immune training.
Medications: broad-spectrum antibiotics, NSAIDs, proton-pump inhibitors can alter gut ecology.
Environmental toxins: pollutants and heavy metals can stress the barrier and immune cells.
Understanding these causes is the first step to restoring the gut immune axis — because you can’t fix what you don’t know you’re harming.
Evidence from studies (short, practical summary)
Clinical and preclinical research supports the core idea: gut microbes influence immunity. Examples:
Children with reduced microbiome diversity have higher allergy risk.
Probiotic supplementation reduced incidence/severity of some respiratory infections in some trials.
SCFAs produced by fiber-fermenting bacteria reduce inflammation in the gut lining.
These findings point to a clear reality: the gut immune axis is not just theory — it shows in human and animal studies repeatedly.
Diet strategies to restore a healthy gut immune axis

Diet is the most powerful, practical tool you have to influence the gut immune axis.
1. Prioritize fiber and varied plant foods
Eat a wide variety of vegetables, fruits, whole grains, legumes, nuts, and seeds. Diversity of plant fibers feeds a diverse microbiome. Aim for 25–35 grams of fiber daily. Think colorful plate: greens, orange vegetables, berries, beans.
2. Add fermented foods
Daily small servings of yogurt, kefir, kimchi, sauerkraut, or miso introduce beneficial strains and enzymes. These help rebalance the microbiome and support the gut immune axis.
3. Reduce ultra-processed foods and sugar
These feed opportunistic microbes, reducing overall community resilience. Cutting back supports microbial recovery.
4. Include omega-3 rich foods
Fatty fish, chia, and walnuts reduce inflammation and support immune regulation.
👉 Affiliate suggestion: quality probiotic and fermented food starter kits can help — check this probiotic on Amazon.
• Beyond broad food groups, culinary herbs and spices are hidden allies for digestive health and immunity. Garlic, ginger, turmeric, oregano, and rosemary have bioactive compounds that reduce harmful microbes while nourishing beneficial ones. Turmeric’s curcumin, for example, is studied for its ability to modulate immune pathways and calm chronic inflammation.
Ginger helps motility in the digestive tract, reducing stagnation and bloating. When you incorporate these flavors into daily cooking, you’re not just seasoning meals—you are actively strengthening the gut immune axis. Even small daily amounts add up, and unlike supplements, herbs arrive with the synergy of whole food chemistry.
Lifestyle habits that support the gut immune axis

Diet alone helps a lot, but combine it with daily habits for real repair:
Sleep: aim 7–9 hours; sleep supports immune cell renewal.
Stress reduction: short breathing practices, 10–20 min/day of meditation lowers cortisol and protects the barrier.
Movement: regular walking or light exercise supports gut motility and microbial diversity.
Sunlight: morning sun helps circadian rhythm, which in turn supports microbiome cycles and immunity.
Hydration: proper fluids support mucosal function and digestion.
Each habit sends signals through the gut immune axis toward resilience.
• One often-overlooked factor is exposure to nature. Spending time outdoors—gardening, walking in forests, or simply breathing fresh air—introduces the body to environmental microbes that diversify the microbiome. Modern sterile indoor environments may limit this natural exchange. Studies show children raised on farms or with outdoor pets often have stronger immune tolerance, fewer allergies, and more resilient gut flora.
Adults benefit too: grounding in natural spaces lowers cortisol and supports circadian balance, both of which stabilize the gut barrier. So a simple afternoon in the park is not leisure alone—it is direct nourishment for the gut immune axis.
Supplements: when and what to consider
Supplements can be useful adjuncts when chosen judiciously:
Probiotics: some strains help restore balance and reduce inflammation. Choose multi-strain, clinically-studied products. Check this probiotic on Amazon.
Prebiotics: inulin, FOS, and resistant starch feed helpful bacteria.
Vitamin D: crucial for immune regulation. If levels are low, supplementation helps. Vitamin D supplements on Amazon.
Zinc & Vitamin C: support immune cell function, especially during recovery.
L-Glutamine & Collagen: support gut barrier repair in certain protocols.
Always consult your healthcare provider before starting supplements. Some conditions require specific dosing and oversight.
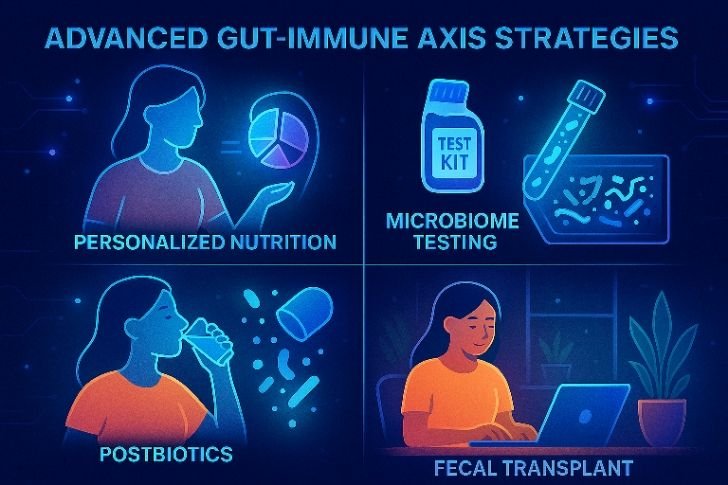
• Emerging research focuses on next-generation prebiotics: specialized fibers designed to feed very specific beneficial strains. Examples include partially hydrolyzed guar gum, galactooligosaccharides (GOS), and human milk oligosaccharides (HMOs, synthesized for adult use). These compounds selectively increase levels of Bifidobacteria and Akkermansia, species linked to reduced inflammation and improved barrier integrity.
Incorporating such advanced prebiotics might not be necessary for everyone, but for people with compromised digestion, they may give the gut immune axis a stronger push toward balance. 👉 Explore advanced prebiotic powders on Amazon.
Practical 30-day plan to strengthen the gut immune axis
Here’s a simple, evidence-informed 30-day plan you can follow to kickstart repair:
Week 1 — Clean baseline
Remove ultraprocessed foods and reduce sugar.
Add one fermented food daily.
Drink 1–2 glasses of water on waking.
Week 2 — Build fiber
Add beans/legumes 3x per week.
Include at least 3 different colored vegetables daily.
Start 5 minutes of daily breathing or meditation.
Week 3 — Lifestyle anchors
Regular sleep window (same bedtime/wake time).
20–30 min movement daily (walk/yoga).
Try a probiotic (choose reputable brand).
Week 4 — Reinforce & monitor
Track symptoms: energy, digestion, mood, sleep.
Add one advanced habit (sunlight in morning, journaling).
Reassess supplements with a clinician if needed.
Small consistent changes create durable improvements to the gut immune axis.
When to see a clinician or specialist
If symptoms are severe or persist — recurrent infections, dramatic weight changes, blood in stool, high fevers, or signs of autoimmune disease — get specialist support. Tests to consider:
stool microbiome analysis (clinical interpretation required)
basic blood panel: CRP, vitamin D, zinc, CBC
celiac testing if applicable
gastroenterology referral for persistent gut symptoms
Advanced interventions (like fecal microbiota transplant) are used selectively, under specialist care; they show promise in some refractory conditions.
The future: personalized gut immune axis medicine
Research is moving from broad recommendations to precision approaches:
Microbiome-guided diets — tailored by stool analysis
Postbiotics — therapeutic bacterial metabolites
Targeted microbiome editing — phage therapy or designer probiotics
Today you can start with diet, sleep, stress reduction, and targeted supplements; tomorrow medicine may refine these with individual data.
Quick FAQs (practical answers)
Q: Will probiotics cure autoimmune disease?
A: No. Probiotics can support balance but they are rarely a cure. They’re best used as part of a broader plan that addresses diet, sleep, stress, and environment.
Q: How fast will I feel better after improving my gut?
A: Some people notice digestion or energy changes within 2–3 weeks; immune resilience and deeper changes take months.
Q: Can I test my gut microbiome at home?
A: Yes, but many commercial tests need careful interpretation. Use results as one data point, not the whole story.
Internal resources & further reading
Leaky Gut Syndrome: Symptoms, Causes, and Natural Fixes — see Pillar article on Leaky Gut
The Hidden Link Between Stress and Gut Inflammation — Cluster: Stress & Gut Inflammation
10-Minute Evening Rituals to Lower Cortisol — Cluster: Cortisol & Sleep
• Consider two practical stories. Anna, a 35-year-old teacher, suffered repeated colds and bloating. By shifting breakfast to oatmeal with flax and berries, adding sauerkraut twice weekly, and improving her sleep, she noticed within 6 weeks that colds shortened and energy returned. John, a 50-year-old desk worker, had autoimmune joint pain.
Under guidance, he removed highly processed foods, added turmeric and fish oil, and started daily walks. Over months, his flare-ups reduced. These are not miraculous cures—they are practical examples of how daily habits tune the gut immune axis. Real change comes not from a single pill but from many consistent steps working together.
Conclusion — Treat the gut immune axis as your inner guardian
If you want a stronger immune system, don’t start with pills alone — start with the gut. The gut immune axis is the frame that holds immunity together. Feed it with fiber, nurture it with fermented foods, protect it with sleep and stress practices, and support it with targeted supplements when needed.
Small daily choices — the food you put on the plate, the minutes you give to sleep, the breath you take during stress — all speak to the gut immune axis. Over weeks and months, those choices become the signals that shape whether your immune system stands ready or stands tired.
Start today: add one extra vegetable, go to bed 30 minutes earlier, try a probiotic if appropriate. Each step is a vote for resilience — and the gut immune axis listens.
